For automobile insurance in Florida, drivers are subject to Florida Statute 627.736, which is more commonly known as the “PIP Statute.” This statute requires drivers in the state to carry Personal Injury (PIP) Coverage which entitles those injured in a car accident to coverage of medical treatments and lost wage, regardless of who caused the accident.
It’s a unique law that is unlike any other state, and it also means that many individuals – from drivers to chiropractors to lawyers and more – are still trying to fully understand not only how the law works, but how they can follow it successfully and in the best interests of all parties involved.
TeleEMC offers a telemedicine service, here in Florida, that partners with chiropractors and lawyers to improve the PIP approval process. For chiropractors, we provide EMC determinations remotely, with same day service that can be completed from your office. We can also schedule EMC appointments on demand, while the patient is at your office, depending on time and availability.
We also have a network of PIP attorneys to help handle legal issues for our chiropractor partners, and for attorneys that we are not partnering with, we can provide you with rejected approvals to help you move forward with your legal services.
You can learn more about TeleEMC and how we help chiropractors and personal injury lawyers by calling us at:
866-611-4EMC (4362)
About the PIP Statute
We’re different here in Florida. From our weather to our people, Florida is unlike any other state. So it’s not surprising that we also have laws that may differ from those in other areas, and often – even for those that pay close attention to the politics of auto insurance – applying these statutes can still have its complexities.
Before we start to explore the Personal Injury Protection Statute from a professional perspective, it’s best to start with the basics: what it is, and what it means for the average, everyday driver.
How the Florida PIP Statute Affects Drivers
Florida Statute 627.736 was passed in 2012, and became law in 2013. It is a law that requires drivers to carry what’s known as “Personal Injury Protection” insurance, that provides both medical coverage and “loss of work” coverage, no matter who is at fault for the accident.
Coverage under the PIP Statute entitles those injured in a car accident to a maximum of $10,000, or 80% of the total cost of medical costs, whichever is less. This insurance covers the driver, passengers in the car at the time of the accident, and relatives living in the insured driver’s household. It also covers those struck by a motor vehicle who then require medical care.
The PIP statute was passed with the intent to provide those injured in an accident with immediate medical coverage. Prior to this statute, claims could be delayed while insurance companies and the courts established who was at fault, and therefore liable, for the accident.
What Does PIP Insurance Cover in Florida?
All drivers in Florida must carry PIP insurance as part of their policy. PIP insurance provides coverage for medical expenses and lost work income that results from an automobile accident, no matter who was at fault.
Under the driver’s policy, the insurance coverage applies to the driver, any passengers in the car during the accident, and any relatives living with the driver.
Emergency Medical Condition | Medical Benefits and Coverage
PIP insurance covers 80% of medical expenses up to $10,000 when a doctor diagnoses an emergency medical condition caused by an accident. When a patient seeks medical attention but is not diagnosed with an emergency medical condition, this coverage provides up to $2,500 in reimbursements.
If an auto accident injury causes a person to be unable to earn a living, PIP insurance provides disability benefits. These cover 60% of:
- Gross income lost from not working.
- Earning capacity when an individual cannot earn a living in the future.
- Services the injured person would have performed for their household if they were not injured but must now be performed by a hired person or business, such as housework.
In addition to medical benefits and lost income coverage due to a disability, the insurance provider can pay out death benefits of up to $5,000 per individual deceased as a result of the accident.
Receiving Medical Care Within 14 Days
An important part of the statute, an one of the few that isn’t in favor of the patient, is the PIP 14 day rule. This rule requires that those injured in an auto accident seek necessary medical treatment within 14 days of the accident in order to qualify for coverage. Waiting to seek treatment for any reason, even if it is because the pain does not occur right away or you’re unable to get any help, means that you cannot receive any PIP coverage.
Seeking medical coverage means receiving services from a licensed medical provider for a condition that resulted from the accident. These medical providers include:
- Physician
- Dentist
- Chiropractor
- Registered Nurse
- Emergency Medical Services (Paramedics and Ambulatory Transportation)

Additionally, services received in a hospital or emergency room qualify as care so long as they are received within 14 days and related to the accident.
The PIP statute also covers ongoing medical care that occurs after the initial 14 days, such as continuing treatments, surgeries, and physical rehabilitation, as long as they are referred by one of the above medical providers.
Of the covered services, massage therapy, acupuncture, and unknown experimental alternative treatments are not considered medical care under the statute. This is the case regardless of who is administering the massage or acupuncture – even if administered by a chiropractor.
The 14 day rule is perhaps the most important rule that patients, attorneys, and medical teams need to keep in mind when determining whether or not a patient will qualify for PIP funding.
The second most important rule, however, is the EMC designation.
The Necessity of the Emergency Medical Condition Designation
It’s here where TeleEMC – and, potentially, you – starts to become more important. We’ll have more on our services later in this guide, but this is where the law becomes more difficult for all parties involved.
In order to qualify for the entire $10,000 of coverage, the injured person must receive a diagnosis of an emergency medical condition as a result of the car accident.
These diagnoses can be performed by a qualified doctor, dentist, or nurse practitioner and includes diagnosing that the patient has symptoms, including pain, that reasonably result from or may cause the following if not treated immediately:
- Risk to the health of the patient.
- Risk to the bodily functions of the patient.
- Risks to the bodily organs of the patient.
The emergency medical condition does not need to be diagnosed within the first 14 days following the accident as long as medical treatment was sought during that time. Treatment is also not limited to that time frame. If the person has received any treatment within the first 14 days, the diagnosis of an Emergency Medical Condition would still be valid even if it occurred later in treatment.
A diagnosis of such a condition at any time makes the patient eligible for up to $10,000, or 80%, of coverage for medical expenses, whichever is less.
When medical care is sought within 14 days, but there is no diagnosis of an emergency medical condition, the injured person can only receive up to $2,500 in benefits.
Time is clearly of the essence for the patient, who is in pain, but may be hesitant or afraid to get treatment not knowing if their care will be covered by the law.
TeleEMC provides 100% virtual EMC designations by experienced local doctors that are licensed to provide these recommendations. We partner with chiropractors across the entire state of Florida to:
- Make sure that patients get their EMC determination fast.
- Make it possible to obtain an EMC determination from the chiropractor’s office.
- Make sure that patients and doctors get what they need to move forward.
Virtual appointments are as legal and valid as any other type of medical visit, and our doctors are always accurate in their determinations, basing it off the latest diagnostic techniques.
Yet there are still insurance agencies that will refuse a valid EMC determination. We want to make this easier on the patient too, which is why we partner with personal injury attorneys to help them recover what belongs to them. We’ll have more on this later in the guide, but wanted to prime you for a better understanding of how we can benefit all parties involved, including you.

PIP Claims in Florida – How the Claims Work
One of the reasons that PIP insurance is so valuable for drivers and chiropractors is that it opens the door for anyone to receive some form of treatment. What makes accidents so challenging is that even the most minor of accidents – one that barely even counts as a fender bender – can trigger conditions that lead to significant pain.
So getting the claims correct is extremely important for the establishment of treatment. Anyone in a car accident of any kind is recommended to immediately visit a medical specialist to first make sure that they establish treatment within those first 14 days.
Chiropractors are allowed to be that first treatment, so it is often recommended that chiros consider marketing themselves to those in accidents, and let them know to contact them immediately to be the first line of care for some non-life threatening accidents.
The $2,500 or $10,000 covered by the PIP apply to any and all payments, including:
- All related medical services, surgery, and medications.
- All related diagnostic services.
- All related hospital stays or ambulance rides.
- 60% of lost wages.
- Most related rehabilitation and recovery costs, excluding acupuncture and massage therapy.
These costs can add up quickly – which is one of many reasons an emergency determination is so important, as without it, the patient may struggle to afford the services with only $2,500 available. Patients are also advised to consider consulting with a personal injury attorney to handle these claims (more on that later), though they are not required by law.
Assuming the patient has received medical care within 14 days, and assuming the patient has both a car and auto insurance, the patient would then file a claim with their own insurance provider. Once the claim has been made, the provider has 30 days to make the PIP payout.
NOTE: TeleEMC bills the PIP ourselves. So patients are not expected to know how to contact the insurance provider or make the necessary applications in order to receive their full amount. Our in-house team takes care of this for the patient, and for the chiropractor, so that the claim can be made correctly and with ease.
Here are some example situations that may occur that affect the patient and the treatment provider:
No Treatment After 14 Days
One situation that patients may find themselves in is not seeking out treatment within 14 days of the initial accident. In these cases, the patient does not qualify for PIP coverage.
However, what qualifies as an “initial treatment” is purposefully fairly broad. Not only is a visit to a doctor in almost any setting (private practice, hospital, etc.) considered an initial treatment, but even an emergency transport would qualify as establishing some type of care within the 14 day period.
Treatment Without First Getting an EMC
You do not need to obtain the EMC right away in order to make a claim for the full $10,000, but the longer a patient waits, the more challenges there can be. First, the treatment that a patient is receiving may not be covered without the EMC, putting both the patient and the provider at risk for financial challenges. Second, a patient receiving an effective treatment may start to recover before the EMC determination has been made, at which point it may become more difficult to make a proper, legally valid EMC determination.
Patient Receives EMC, But Claim is Denied
If the patient has received treatment within 14 days, and they have received an EMC, insurance companies can and have historically tried to fight the claim in order to avoid making the $10,000 payoff. The law is on the patient’s side, however, although in some cases the patient may need to get in touch with a personal injury attorney (which TeleEMC partners with). So, in the event that a claim was denied, the attorney will be able to come in with all of our information and supporting documents and help the patient obtain the $10,000 fee.

Traditional EMC Process for Chiropractors

Chiropractors are allowed to be the first (and only) treatment that patients receive, if that is all that is needed for their care. Patients can contact a chiropractor immediately after an accident and have that specialist see their injury and determine the best course of treatment.
But chiropractors are at one disadvantage compared to other medical specialists: Most are not allowed to make EMC Determinations.
That’s a challenge that has caused problems for a lot of chiropractors. It means that in order for patients to receive the full PIP payout amount, their chiropractor has to make a referral to a medical specialist that can provide the necessary diagnostics. That has often created issues:
- Scheduling – Patients are generally in a hurry. They’re in pain, and they need to have a better understanding of whether or not their care will be covered by the PIP. If the specialist is unavailable for a while, or there are scheduling conflicts, the patient may have to wait before they get the diagnosis, increasing their stress and discomfort.
- New and “Bad” Experience – Sending someone out to a specialist means that they’re going to have a new, separate experience from being in your office – one that is out of your control, but be attributed to their workplace, possibly decreasing their satisfaction with your service. In an era of COVID-19, it also increases the amount of in-person contact they have with others.
- Bias in the Specialist’s Recommendation – There’s a saying in the medical community. Whatever type of doctor you see, that’s what you’re diagnosed with. No matter what the problem is, if you see a dermatologist you have a skin condition, a neurologist and you have a brain condition, and so on, even if you’re seeing them for the same ailment. Similarly, if you send a patient out to see someone for an EMC determination, there’s a risk that the person they see will recommend a different service than the one you’re providing.
These are only a few of the different challenges that both patients and chiros may face when they’re forced to send patients out to get their EMC determinations.
Of course, that’s the traditional way. The new way is with TeleEMC, where we have experienced physicians that provide EMC determinations online, and can take place within your office, often on the days that the patient is already scheduled to be there for your service. It’s fast, convenient, becomes a part of your business, and is unbiased in treatment recommendations.
Still, the traditional process has been able to provide chiropractors with the approvals they need for patients to receive the full Florida PIP amount.
PIP for Lawyers – How Attorneys Can Benefit from PIP (and TeleEMC)

Attorneys play an important role in the PIP, even more so than personal injury attorneys in many other states. That is because there are many situations a patient may find themselves in where a legal advocate is important for them to get the care they need. Some of these situations include:
- Insurance Company Denies PIP Claim – Once a patient has received an emergency medical condition declaration from TeleEMC or elsewhere, insurance companies are expected to pay it. Some may deny the claim, or try to claim fraud, in order to prevent the payout. But in the vast majority of situations, the insurance company is required to make this payment, which means that a denied claim can be taken up by the personal injury attorney.
- Insurance Company Takes Too Long – According to the 627.736 Florida PIP statute, insurance companies are required by law to make the PIP payment within 30 days, even if they suspect (or claim to suspect) that the patient is committing fraud. An insurance company that is delaying payment is violating this law, and a personal injury attorney can be a helpful tool in addressing this on behalf of the patient by suing in favor of the PIP payout.
- Medical Costs > $10,000 – Florida is one of the few no-fault states that allows patients to file suit if the medical bills will be greater than $10,000. This is also only possible if the patient receives the EMC (and thus approval for the full amount of the PIP payout), and it requires a lawsuit which can be taken up by the Florida PIP personal injury attorney.
These are some of the scenarios where an attorney is necessary and valuable, and in many cases, you will find that those that are struggling with their injury or their PIP claim will be receptive to the idea of hiring an attorney, especially if the insurance company tries not to pay out for the PIP.
Attorneys that decide to take on PIP claims have to verify a few facts about the claimant before they can file suit against the insurance company:
Does the Patient or Someone in their Household Own a Car?
Those involved in an auto accident do not need to be driving. In fact, they do not need to be in a car at all. If you’re hit by a car while you’re on a bike, for example, your PIP insurance is expected to cover you.
But they – or someone in their family – does need to own a car. Protecting against fraudulent PIP insurance claims is important, and verifying that a car is owned by the patient (or a live-in relative, whose car they may have been driving) is step one.
Is the Car Insured?
PIP is a form of mandatory insurance, so if the car is insured in the state of Florida then it has PIP insurance. But it is important to check, as there are those driving uninsured cars who would not be able to take advantage of the PIP payout, even if they are not personally at fault for the accident.
Does the Driver of the Other Vehicle Have Insurance?
In the event that the patient has no insurance, and does not have anyone in their family that has insurance, it may still be possible to use the PIP of the other driver, especially if that driver is or is likely to be considered “at fault” for the accident.
But that’s about it. Because anyone with car insurance in Florida has PIP coverage, and because that coverage is no-fault, mandatory with a PIP, and have a set payout rate, there are not many requirements that need to be met in order for someone to both qualify for the PIP and qualify for the full payout (with an EMC).
Personal injury law is tricky, especially after a car accident. Still, typically going after a PIP case is a little more straight forward when all the boxes are checked. The law is specifically designed to favor the injured, and so while insurance companies continue to try to skirt around the payout as best they can, attorneys that understand the PIP rules tend to find that they are at an advantage in pursuing a payout, making it easier to take home their contingency with less risk.

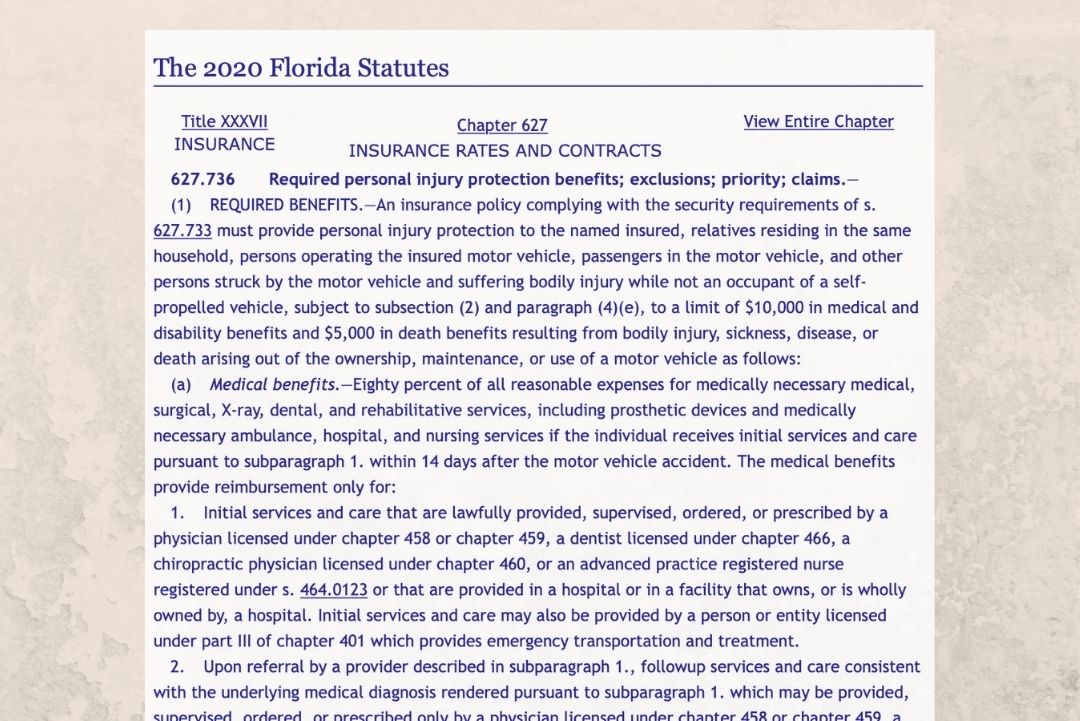
Further Understanding of the PIP Law
For those that are new to the PIP, or would like to gain a further understanding of the legalese found within the law, it is best to visit the Florida State Legislature page for the specific ordinance, Florida Statute 627.736. There, you can read the details of the law, along with all of the amendments and changes since the law has taken effect.
Find the details here.
For attorneys and chiropractors, we’re also happy to answer any questions you have about EMCs and their examinations. You can contact our team at any time by visiting our contact us page.
How TeleEMC Can Help Chiropractors with PIP Claims

PIP claims are an important part of any Florida chiropractor’s business. Both the $2,500 base and the $10,000 EMC claim provide a chance for chiropractors to give the care their patients need without the patient worried about whether or not they can afford it.
But knowing whether a patient is getting the full amount of the PIP is important, because it helps guide treatment, gives providers a chance to know their bills will be covered, and gives patients the piece of mind knowing that their financial needs will be met. The faster and more efficiently you can get that EMC determination, the better.
TeleEMC works almost exclusively with chiropractors. We run EMC diagnostic tests via video, with experienced physicians that are able to use a series of tests to determine if the patient has an emergency medical condition. We provide a free tablet to our chiropractors, who can then have the patient receive the EMC determination in house – right from your office, and even before or after an appointment if scheduled in advance.
The entire process takes 30 minutes with appointments available right away – sometimes same day. This provides many advantages for both patients and their chiro practitioners that need to figure out their PIP status, as it offers:
- Professional Convenience – By giving patients the opportunity to get their EMC determination from within the chiro’s office, it helps the entire experience feel like it is coming from only one business – yours – and reduces the amount of running around or meeting new people that patients would have to do in order to get the determination they need.
- Fast and Ready – Similarly, this determination is critical for knowing how to proceed with treatments, and the sooner that you get it, the better it will be for you and the patient. Because we are often able to schedule appointments that very same day that someone goes to your office, while they’re there, you have a response fast enough that you can make the appropriate decisions with regards to treatment. Once we have completed the exam, we are able to send the results within 24 hours, so patients can keep getting the care they need.
- Accuracy in Reporting – One of the more obscure rules of the PIP is that the EMC diagnostician must specifically use the phrase “Emergency Medical Condition” for the PIP to pay out the full $10,000. Some physicians are not as familiar with this rule, and may not explicitly say that the issue is an EMC, thus complicating collections.
- We Bill the PIP – Our ability to bill the PIP on your and your patient’s behalf reduces the labor and opportunity for error on the part of the patient. It’s also yet another step to save time and investment, seeing a better return when working with TeleEMC.
- Easy to Use Secure Online Portal – EMC determinations sometimes need additional documentation and information. Collaborating on this information is simple. Using eClinicalWorks, a HIPAA compliant cloud-based service, chiros can upload supporting documents like X-rays and charts directly to the system for each patient, thus making it even easier to provide the correct determination.
- All Hardware Included – The purpose of TeleEMC is to reduce the amount of labor that both patients and chiros have to go through in order to process patient claims and address their needs. For us, it’s the details that help us show others our commitment to relieving this excess work, and one of the ways we do that is by sending you a tablet and all the hardware and software you need pre-installed, so that you can get started operating our system.
Every step of the way with TeleEMC is simple and intuitive, even when the EMC requirements and Florida PIP law may not be. It’s why we have become the leading choice for so many chiros in Florida, and why there is so much reason to consider our service.
How TeleEMC Can Help Personal Injury Attorneys

TeleEMC is a service for chiropractors. But we also know how important attorneys are to making sure that each accident victim gets what they deserve. That’s why we also create partnerships with some of the best personal injury attorneys in Florida – those that are looking to grow their practice and find new and simple sources of revenue.
And that’s what it is when you partner with TeleEMC: simple. PIP insurance coverage has multiple safeguards for those that are injured in an accident, including the mandatory 30 day payout even if a claim is being investigated, and the requirement of a PIP payment if an EMC determination has been made.
Attorneys that are looking to build their caseload and revenue with simple, straightforward cases will find themselves a strong partner with TeleEMC. Whenever any of the patients that we’ve determined has an Emergency Medical Condition, but has their EMC determination denied, we supply you with all the paperwork, documentation, and resources you need to help these patients win their case:
- Login to eClinicalWorks (ECW) to get access to all patient data.
- All background information about the patient.
- Access to all patient documentation. These include progress notes, uploaded patient medical documents, medical summaries, appointment logs, consultation notes, diagnosed problems, forms, and more.
- In-house advocate you can contact for information related to the EMC determination by our doctors.
- Billing information to help with your case, including outstanding billing.
The attorneys we’ve partnered with in the past agree that it is a simple, effective way to earn revenue, with minimal paperwork and a flat fee, non-negotiable rate. You obtain your contingency fee of the $10,000 PIP settlement, all in a way that is backed consistently by the courts.
Though not applicable for every case, attorneys also find that with TeleEMC, they are able to connect with those of whom might have an additional case beyond the PIP payment, especially if the injury is more severe. By becoming a partner of TeleEMC, you gain the ability to increase your case load with minimal investment in marketing and lead outreach.
Contact TeleEMC for Information to Help Your Practice
Your business depends on making smart decisions that help encourage growth and make it easier to find and treat those that have been in vehicle accidents. Every decision you make – from your chiropractor marketing or your attorney ads that you purchase – is one that is expected to help you manage growth in your practice.
When we developed the idea for TeleEMC, we believed that the most important thing we could do was provide a service that would improve the success of your business, while also offering something that patients (and healthcare providers) genuinely need – access to an EMC that removes all the red tape, prevents speedbumps, and speeds up the entire diagnosis and treatment process.
TeleEMC is the only specialty telehealth medical service that is aimed explicitly and exclusively at providing services that assist both chiropractors and personal injury attorneys with their growth, and do so in a way that helps car accident patients as well.
For Chiropractors: Our service makes it possible for you to improve your services, increase the payout, and offer more to the patient in a way that makes them grateful for your care. We have partnered with hundreds of chiropractors across Florida, and our services can help your business grow and thrive in ways that will make you the top choice in your local area.
For Attorneys: We provide “easy” client work that can provide a healthy chunk of revenue, all for what should be – at least in most cases – minimal work compared to other legal services. We know how difficult it can be to obtain a steady flow of clients with decent profit potential, and we are happy to use our documentation and services to send individuals your way when their case deserves attention.
We have a state of the art system that is use by those across the state, and in an era of COVID-19, we are one of the safest ways to conduct business for both providers and patients. Learn more about TeleEMC by contacting us today at (866) 611-4EMC, or by watching our introductory video.

Florida PIP and EMC FAQs
Q: Do You Approve All Patients?
A: We take our role seriously, and give each patient a thorough evaluation in order to determine if they have an emergency medical condition. We’ll let you know our determination within 24 hours, so that you can coordinate with the patient. If we determine the patient does not meet the criteria, we will let you know, and if they do, we will make sure all of the paperwork is in place for their insurance claim.
Q: How Much Does an EMC Evaluation from TeleEMC Cost?
A: We do not charge chiropractors for our services. We bill insurance companies just as we would for any other type of medical service.
Q: Do Insurance Companies Accept TeleMedicine Exams for PIP Payouts?
A: Yes. Insurance companies accept online appointments and have since 2006. Florida law (Rule: 64B8-9.0141 of the Florida Department of Health) also verifies that they are as accepted a form of medical examination, and would be supported in court.
Q: What Happens if the Insurance Company Suspects PIP Fraud?
A: Fraud with the PIP is difficult, if not impossible, with the TeleEMC medical exam, as we are extremely thorough. Patients also have many rights and support when it comes to insurance company payouts. Even if an insurance company suspects fraud, or claims to suspect fraud, they still have to make the payment within 30 days, and they have to complete their fraud case within 60 days from the date of the claim.
Q: I’m An Attorney. How Often Will You Send Me Cases?
A: It’s too difficult to answer this question, as there are so many different factors involved. But if you’d like to get a basic idea how often we’re referring cases, contact us, and we’re happy to walk you through what our selection process is like. We handle thousands of cases a year, and you know how insurance companies can be.
Q: The Patient Thinks They Have an EMC Already. Do I Still Need Your Services?
A: There are situations where you may still need us to provide an EMC determination. That’s because, depending on the medical care, most doctors are not looking to see if a patient qualifies for an EMC – they’re just checking the patient’s health. They may have found an emergency medical condition, but they may not have explicitly said that the patient has an EMC. It is strongly encouraged within the law that the patient be diagnosed with an EMC, and that the EMC be clearly labeled as such within the paperwork. Call us if you or the patient are not sure if they have already received an EMC.
Q: The Patient’s Pain or Discomfort is Minor. Is it Worth Getting Them An EMC?
A: Almost always, yes. The cost for the visit is billed to the PIP anyway, and thus not paid out of pocket. And the entire purpose of EMC determinations is to see if there is reason to be concerned about patient health or recovery without treatment. Given the difference in both treatment and payout between $2,500 and $10,000, and because determining an EMC is important for the general care and health of the patient, it is almost always recommended that you schedule an EMC determination.
Q: How Long Do EMC Determinations Take?
A: When visiting a typical medical provider, the examinations depend on if the provider is looking at other issues outside of the EMC scope, and other extraneous variables such as the number of patients they have to see and other wait periods. At TeleEMC, our examinations take 20 to 30 minutes, with essentially no wait time from the scheduled appointment start time.
Q: Are the Doctors Reputable and With All Required Certifications?
A: Yes. Every doctor we use is highly regarded and an established name here in Florida. You and the patient can feel confident that your needs are being addressed and that your final determination will be accurate.
Q: Is There Any Way For Patients to Receive the PIP if They Didn’t See a Doctor in 2 Weeks?
A: Unfortunately, no. The law is ironclad here, even in the event that the pain did not arise right away. It’s why anyone in any form of accident is recommended to see a doctor immediately, even if they do not experience pain, to ensure there are no health issues and to establish a timeline for treatment.
Q: Is There Any Way to Get PIP Coverage if the Person Has No Car or Insurance?
A: It depends. Those that live with a relative that has PIP coverage may be eligible. In addition, it may be possible to utilize the PIP coverage of the at-fault driver, even though the PIP is a no-fault insurance. This is a situation where speaking to a personal injury attorney will be helpful to see if you both have a case and if the payout from the case is worth going for.
Q: When is the Best Time to Get the EMC?
A: EMCs can be completed at any time. There are situations where getting additional documentation and diagnostics may be valuable for establishing an EMC – for example, when a case is a bit more complex and an MRI is needed before an EMC can be determined – but our team here at TeleEMC is highly experienced at diagnosing Emergency Medical Conditions, and so our team can schedule the service as soon as they’ve contacted your office.
Q: When Can the Patient Get the EMC?
A: As long as the patient received medical care within those first 14 days, there is technically no specific date an EMC needs to be completed. Patients can complete the EMC weeks or even months later. The law does not specify a mandatory date. However, the longer a patient waits to get an EMC, the more issues there may be with treatments, payouts, and more. In some cases it may even be more challenging to diagnose an EMC if the patient has received treatment first and started to recover as a result. So early diagnostics is helpful for all parties involve.